Groin Itch
Extramammary Paget’s disease (EMPD) often appears as a scaly, itchy or red area within the genital region. The cancer is extremely rare, generally slow growing, and is often misdiagnosed as eczema. The prognosis and recovery from EMPD is often good, especially if it is found and treated early. However some cases of EMPD can be more aggressive, invading the dermis and subcutaneous tissue.

Genital Area Redness
Extramammary Paget’s disease (EMPD) is a rare skin cancer that can appear around the genitalia, groin and perianal regions. If you have redness or a rash that won't go away in these areas, you are encouraged to visit a doctor.

EMPD Cancer
Extramammary Paget’s disease (EMPD) sometimes appears in a similar fashion to “jock itch” around the vulva or anus in women and in extremely rare cases around the penis, scrotum, groin and perianal region in men. In other cases it is often misdiagnosed as eczema.

EMPD Rash
A rash in the genital region is not always just a rash. While extramammary Paget's disease (EMPD) is rare it can spread if left unchecked.

Mohs Surgery
Mohs micrographic surgery is a unique surgery technique that was created by Frederic Mohs in 1938. A Mohs surgeon typically examines tissue under a microscope during or following the procedure.

EMPD Can Spread
In limited cases, extramammary Paget’s disease (EMPD) can spread to areas outside the genital region.

EMPD Can Appear In Many Locations
Typically extramammary Paget’s disease (EMPD) will appear in the genital, anal or arm pit areas in women and men. However, in the rarest of rare cases it can appear elsewhere such as the buttocks, thigh, leg, arm, eyelid, scalp, nose, temple and external auditory canal. In this photo EMPD appears on the arm.

Finding EMPD
Taking multiple 'scouting' biopsies is often a precursor to extramammary Paget’s disease (EMPD) surgery. Biopsies can help physicians understand the extent of the EMPD.

EMPD Documentation
Documentation of rashes or skin discoloration can be helpful in determining if extramammary Paget’s disease (EMPD) is spreading. Photographing these areas can be useful to your physician as they determine the diagnosis and ultimate treatment.

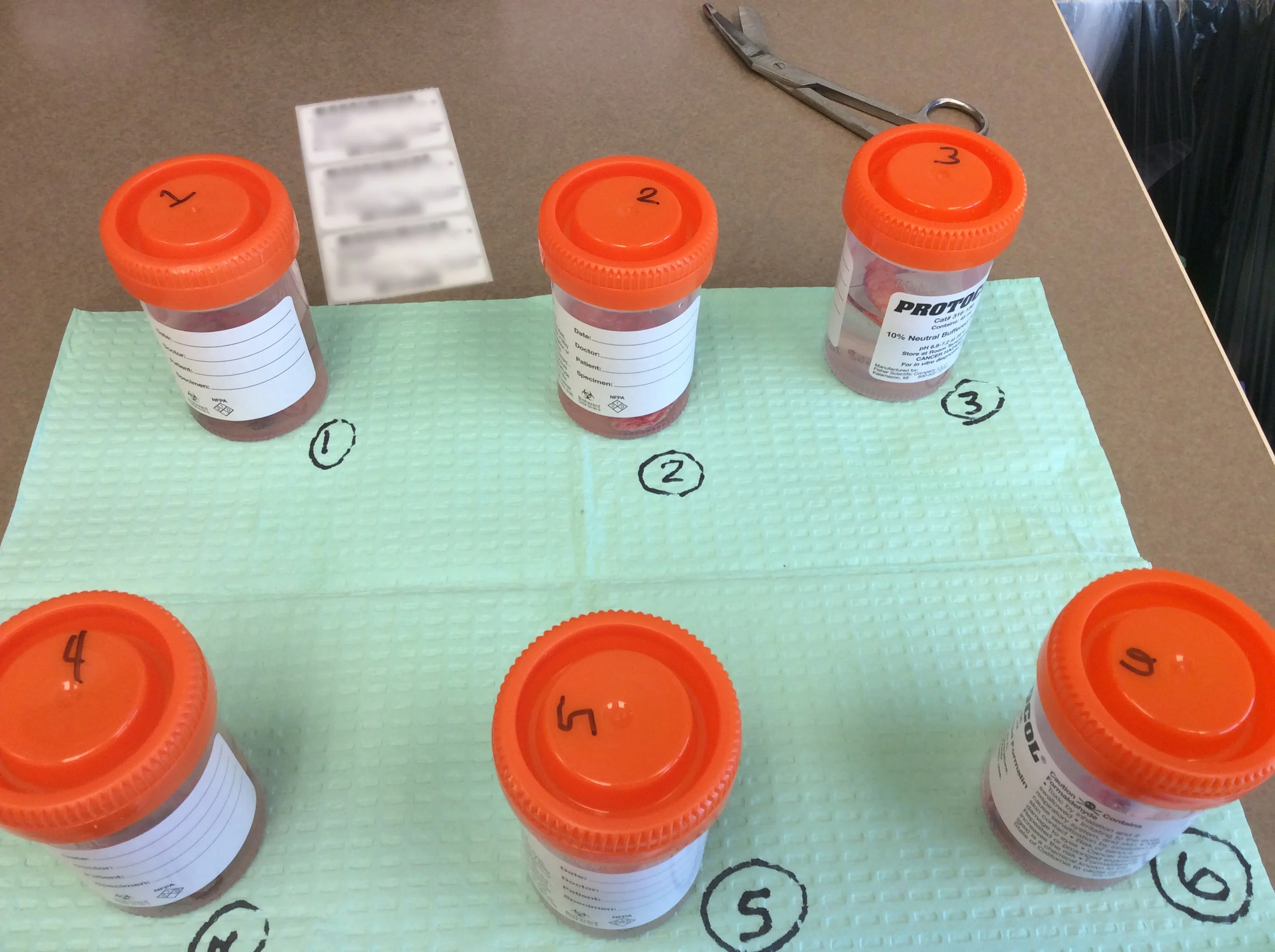
Mapping EMPD Biopsies
Biopsies are a key factor in finding extramammary Paget’s disease (EMPD). Pathologists then play an important role in examining tissue to determine if you have EMPD.

EMPD Surgery
Local anesthesia is often used with Mohs micrographic surgery. During Mohs surgery, the physician will generally use a microscope to exam tissue being removed, thereby reducing the guesswork in the procedure.
Slow Mohs is a modified form of Mohs micrographic surgery and is often used in EMPD treatment. Slow Mohs also involves a margin-controlled excision but the samples are sent to a pathologist, with rush orders, rather than being reviewed in the surgical suite by the Mohs surgeon. Slow Mohs is often used when the tumor has histological subtleties or when a substantial amount of tissue is expected to be removed. The technique requires detailed communication between the Mohs surgeon and the pathologist.

EMPD Exam
A comfortable exam room reduces the stress associated with an extramammary Paget’s disease (EMPD) examination.

In vivo confocal microscopy
In vivo reflectance confocal microscopy (RCM) is a non-invasive imaging technique that allows pathologists to view skin conditions in real time. In the case of EMPD, confocal imaging can help cover a larger area than individual biopsies.
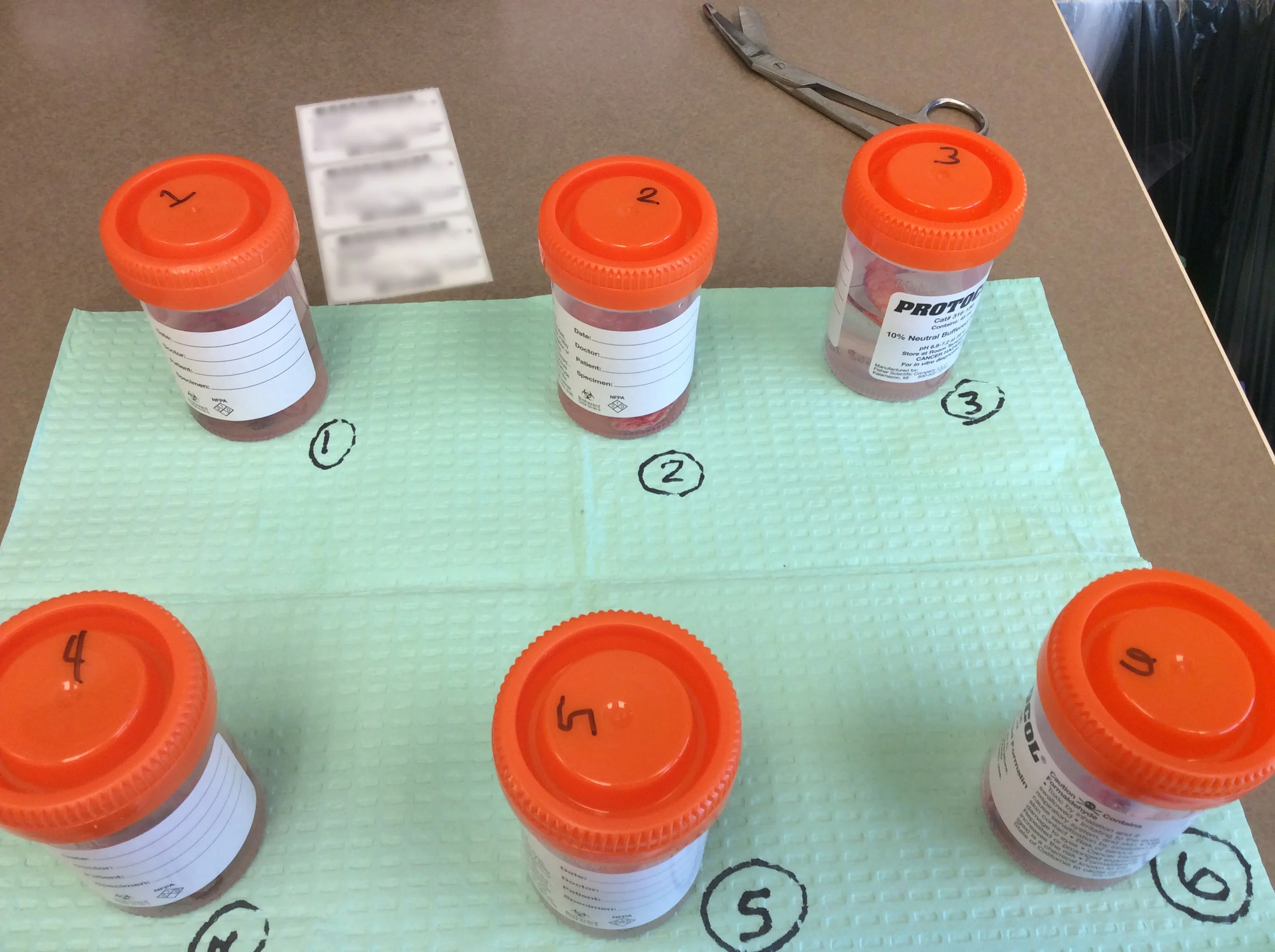
EMPD Tissue Samples
Labeling and tracking tissue samples is a key to tracking extramammary Paget’s disease (EMPD). This process is often used with slow Mohs.
Slow Mohs is a modified form of Mohs micrographic surgery and is often used in EMPD treatment.

Mohs Surgery
Mohs micrographic surgery is often used in treatment of extramammary Paget’s disease (EMPD) when the area of EMPD is confined.

EMPD Is Not Always Obvious
Extramammary Paget's disease (EMPD) can be difficult locate and is not always visible to the eye. In this case In Vivo Reflectance Confocal Microscopy (RCM) was able to find the EMPD in the inguinal fold (as highlighted by the white circle). It was later verified by a traditional punch biopsy.